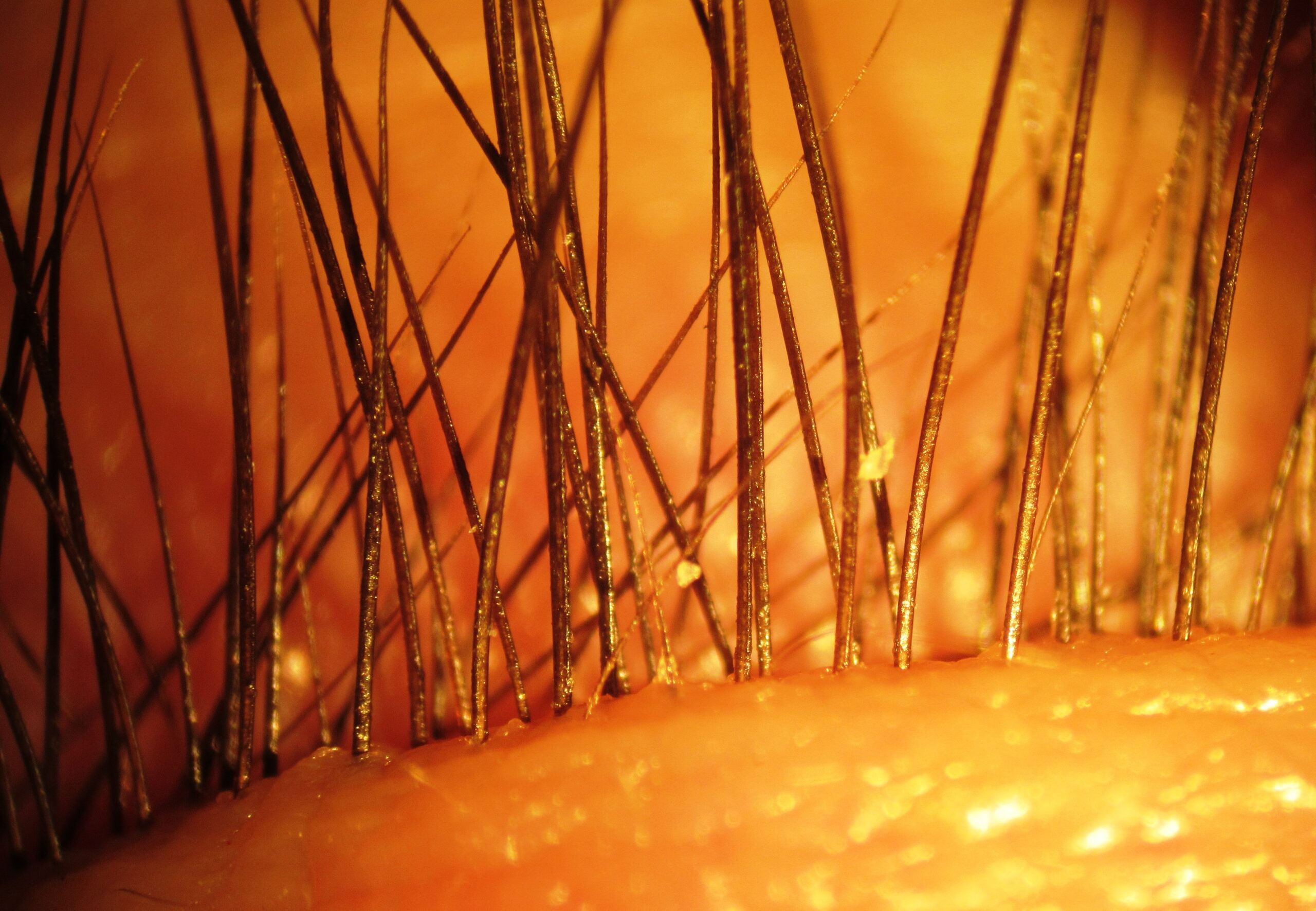
In the second instalment of the Slit Lamp Leries, Martin Conway looks at Oblate Cornea. You can read the previous article which examined Demodex Mites here.

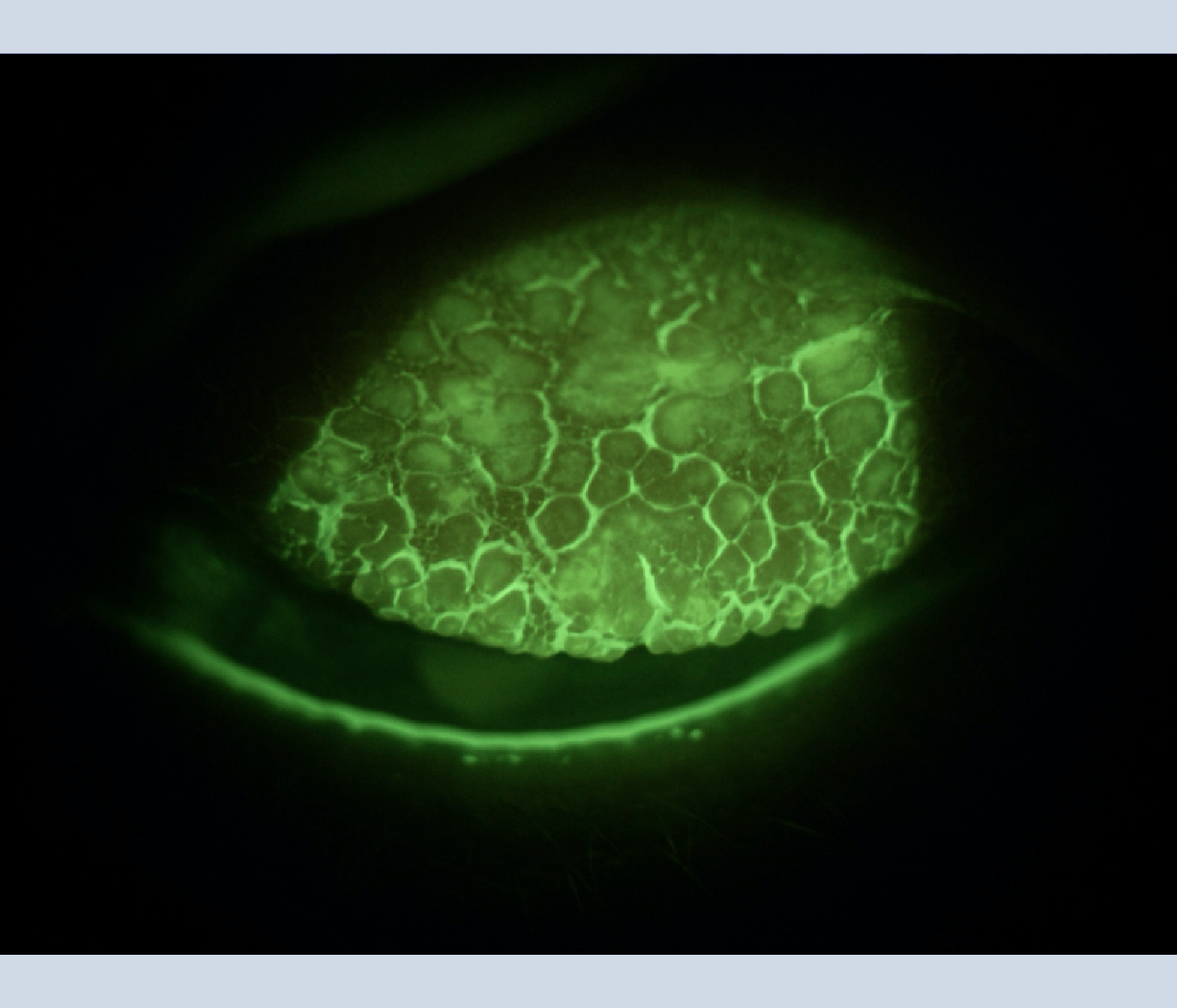
This month’s image from Marco Tovaglia won the BCLA Diane Gould Photo Contest in 2021.
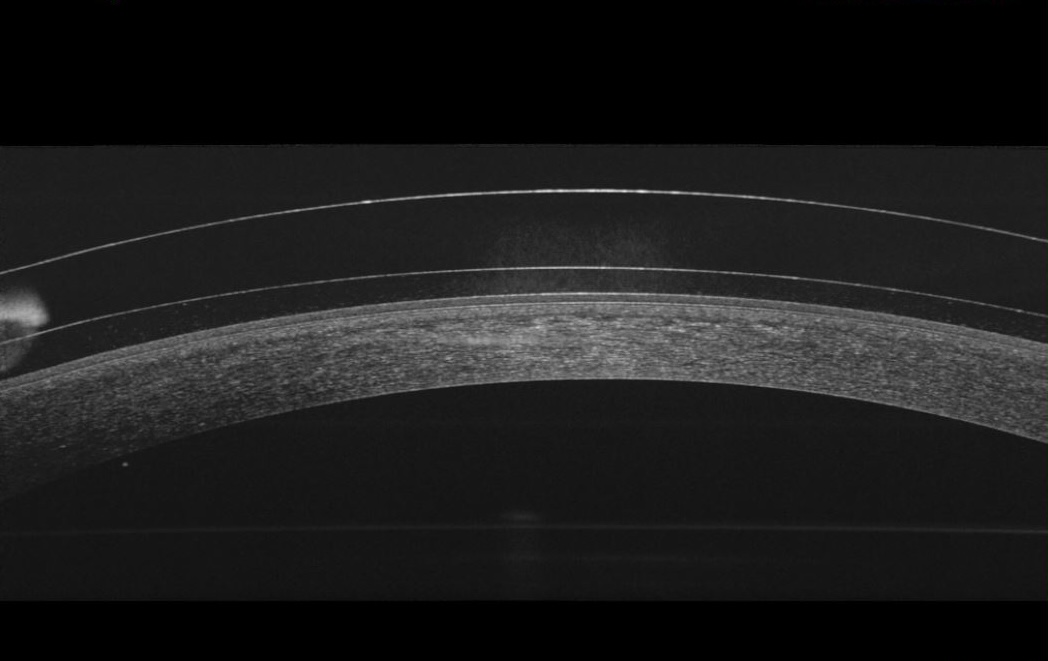
It very clearly illustrates the flattening of the central cornea that occurs following Laser surgery for myopia.
Whilst the aim of such a procedure is to eliminate the need for a correction, there are occasions when the contact lens practitioner is required to correct a residual error caused by the corneal shape changing post-surgery.
There are unique challenges facing the practitioner when presented with such a situation.
Myopic correction will result in the corneal shape becoming flatter in the treatment zone, which will typically be around 8mm. The cornea will then steepen from the edge of the treatment zone towards the limbus, which is the opposite to that of a normal cornea.
Surgeries of this type also invariably invoke some corneal nerve injury during the construction of the flap. The impact of this can range from mild discomfort to neurotrophic corneas.
The resulting desensitisation of the central cornea caused during the construction of the flap may result in reduced innervation to the lacrimal and blink reflexes. In turn, these may result in reduced tear and meibomian gland output.
Case of Oblate Cornea post Laser Eye Surgery
Astigmatic errors, sometimes irregular, are not uncommon.
Last, and by no means least, is dealing with the patient’s expectations. They will be disappointed that their surgery has not given them the result that they hoped for, but this may not have dimmed their expectations. The practitioner needs to address this before attempting to fit and warn the patient that this might require multiple visits and lenses.
Having said all this, these can be interesting and satisfying cases to resolve.
Choice of lenses
For the myopic eye with an oblate cornea, then scleral lenses are the obvious solution, with possibly an oblate design optimising the fit, the tear reservoir can then be supplemented with a wetting agent to cope with any dryness.
Although less common, a hyperopic patient may have a central irregularity, but the remainder of the cornea follows a conventional prolate curve, and so a large diameter GP may be a lens of first choice, possibly with a central zone akin to that of an early keratoconic patient.
In light of these challenges, it’s essential for eye care professionals to conduct thorough pre-fitting assessments, educate patients about potential issues, and tailor their approach to each individual’s unique post-surgery characteristics to achieve the best possible contact lens fit and visual outcome.