Introduction
Limbal stem cell deficiency (LSCD) results in dysfunction and/or loss of the stem cells in the basal limbal area. These cells are responsible for maintaining and replenishing the corneal epithelium. This change in corneal tissue composition results in conjunctival epithelial ingrowth, persistent epithelial defects, chronic inflammation, and neovascularization.1,5 There are numerous conditions that lead to LSCD, and studies have found that about 15% of cases are a result of contact lens wear.4 Literature suggests that this may be due to mechanical trauma resulting from inadequate lens movement leading to increased friction, compression, and hypoxia. This case report aims to explore the use of scleral lenses to treat LSCD when conventional treatment measures do not improve a patient’s ocular surface.
Case Presentation
A 16-year-old female was referred by the corneal specialist for a scleral lens evaluation due to LSCD of the left eye. The patient participated in a monthly soft contact lens research study for six years and is believed to have developed LSCD secondary to the soft contact lens wear.
Chief complaint: blurred vision, light sensitivity, burning and excessive watering OS
Ocular history: LSCD OS, Myopia OU, Astigmatism OS
Ocular surgeries: None
Ocular medications: Artificial tears prn
Right | Left | |
Visual Acuity (cc-gls) | 20/20-1 | 1.0 | 20/80-1 | 0.25 |
Intraocular Pressure | 21 mmHg | 21 mmHg |
External | Normal | Normal |
Lids/Lashes | Normal | Normal |
Conjunctiva/Sclera | White and quiet | White and quiet |
Cornea | Clear | Peripheral whorl-like haze extending from limbus – greatest superior, scattered punctate epithelial erosions |
Anterior Chamber | Deep and quiet | Deep and quiet |
Iris | Round and reactive | Round and reactive |
Lens | Clear | Clear |
Table 1. Entrance Testing and Slit Lamp Examination
Methods and Results
Initial Treatment Plan Prior to Referral:
Discontinue contact lens wear OU
Dry eye management OU
Preservative free artificial tears QID OU
Doxycycline 100mg BID x 7 days
Maxitrol QID OS
Alaway BID OU
Contact Lens Fitting:
OD: discontinue wear of monthly contact lens and refit into daily disposable soft contact lens
OS: fit into BostonSight® SCLERAL 16.5mm with a SmartChannel™
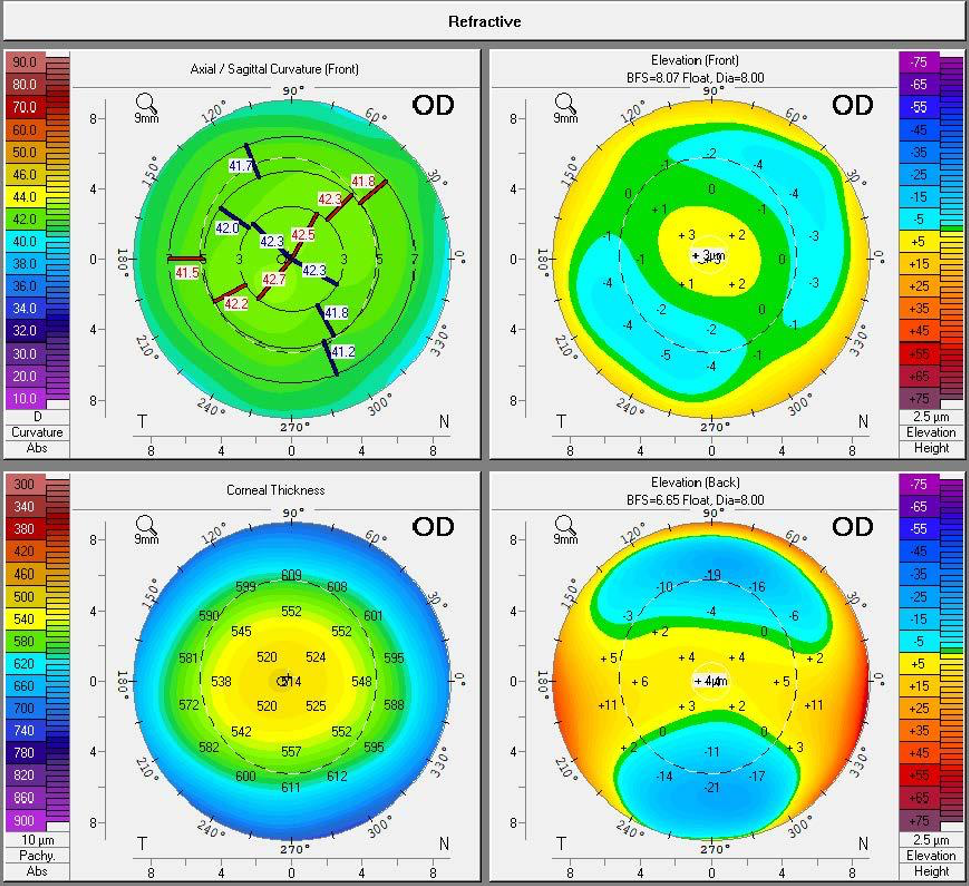
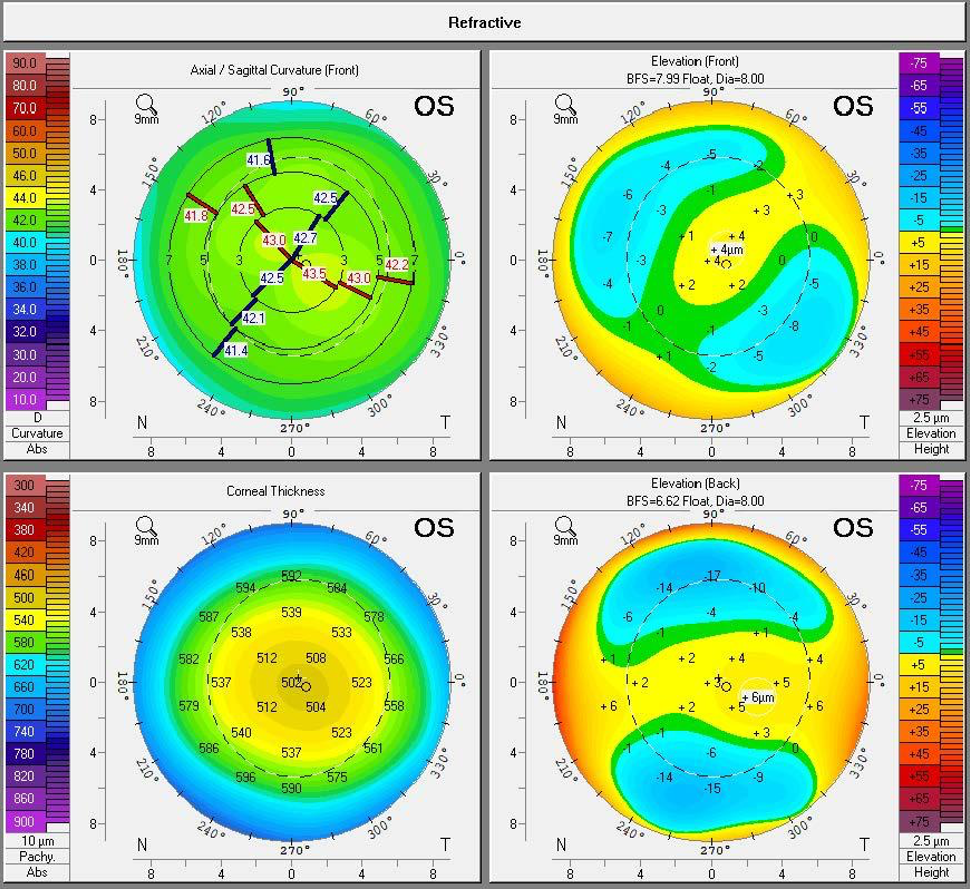
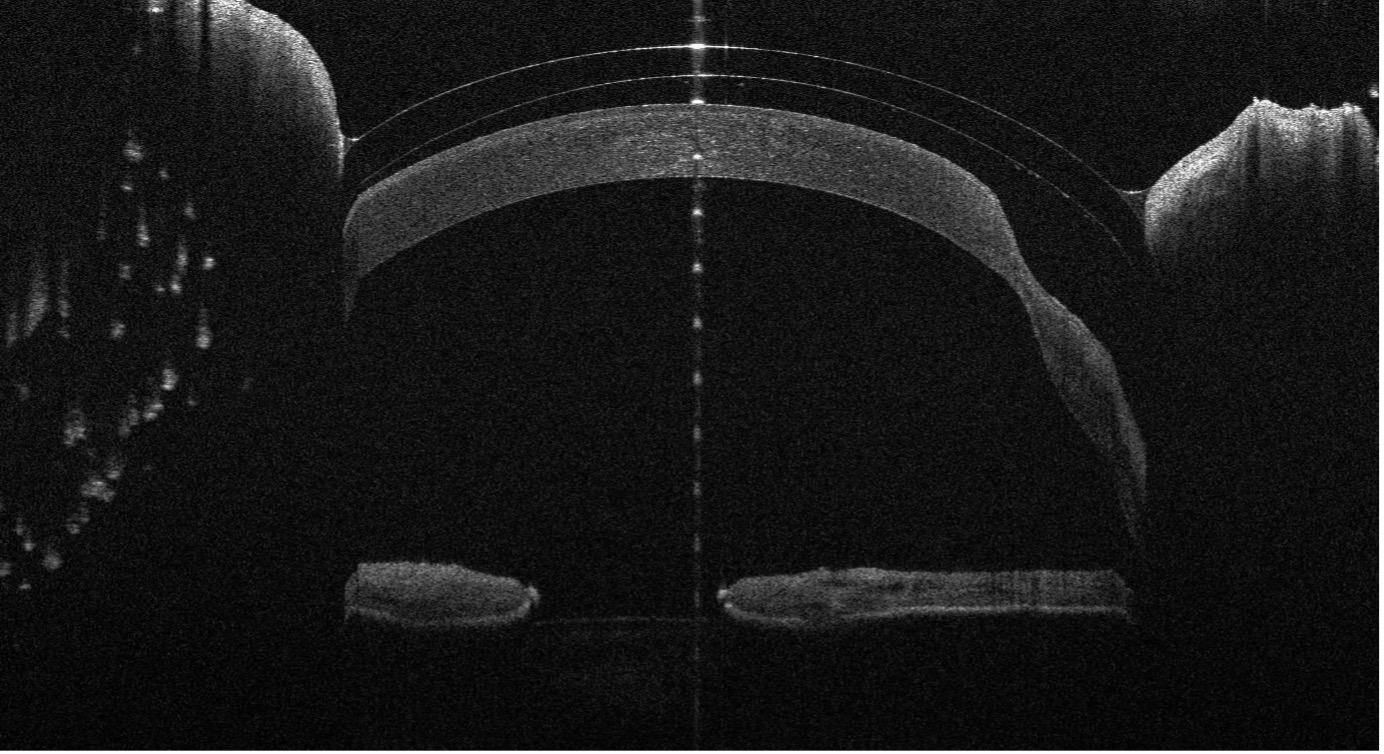
Figure 1. Scheimpflug tomography of the patient’s right and left eye taken prior to contact lens fitting.
Clinical Outcomes:
OD:
- BCVA: 20/20
- Well centered fit with adequate coverage and movement
- No staining upon lens removal
OS:
- BCVA: 20/20-
- Complete resolution of whorl like peripheral haze after 2 months of wear, residual haze at the superior limbus
- No staining upon lens removal
Eye | Brand | Lens | Base Curve | Diameter | Power | Material | Center Thickness |
OD | Alcon | Dailies Total 1 | 8.50 | 14.1 mm | -4.00 DS | Delefilcon A | n/a |
OS | BostonSight® | BostonSight® SCLERAL for Daily Wear | 8.00 | 16.5 mm | -1.48 DS | Contamac Optimum Infinite with Plasma | 0.300 |
Table 2. Final Contact Lens Parameters
Eye | Sphere | Cylinder | Axis | BCVA |
OD | -4.25 | -0.50 | 100 | 20/20 |
OS | -4.00 | -0.75 | 057 | 20/20-1 |
Table 3. Final Manifest Refraction After 5 Months of Scleral Lens Wear
Discussion
Scleral lenses are an excellent management option for LSCD because they provide constant lubrication allowing the cornea to regenerate with minimal disruption. Scleral lenses protect the corneal surface from environmental stressors such as the mechanical trauma that may occur due to the eyelids. Studies have found that the majority of contact lens induced LSCD primarily impacts the superior limbal area. Therefore, superior haptic modifications should be considered to optimize the contact lens fit for these patients.4,5
LSCD can often be misdiagnosed for other conditions. Common misdiagnoses included superior limbic keratoconjunctivitis (SLK), chronic corneal epitheliopathy and corneal intraepithelial neoplasia. Our patient was initially diagnosed with SLK and treated with Maxitrol QID OS. However, SLK is typically bilateral and often has underlying systemic associations.4
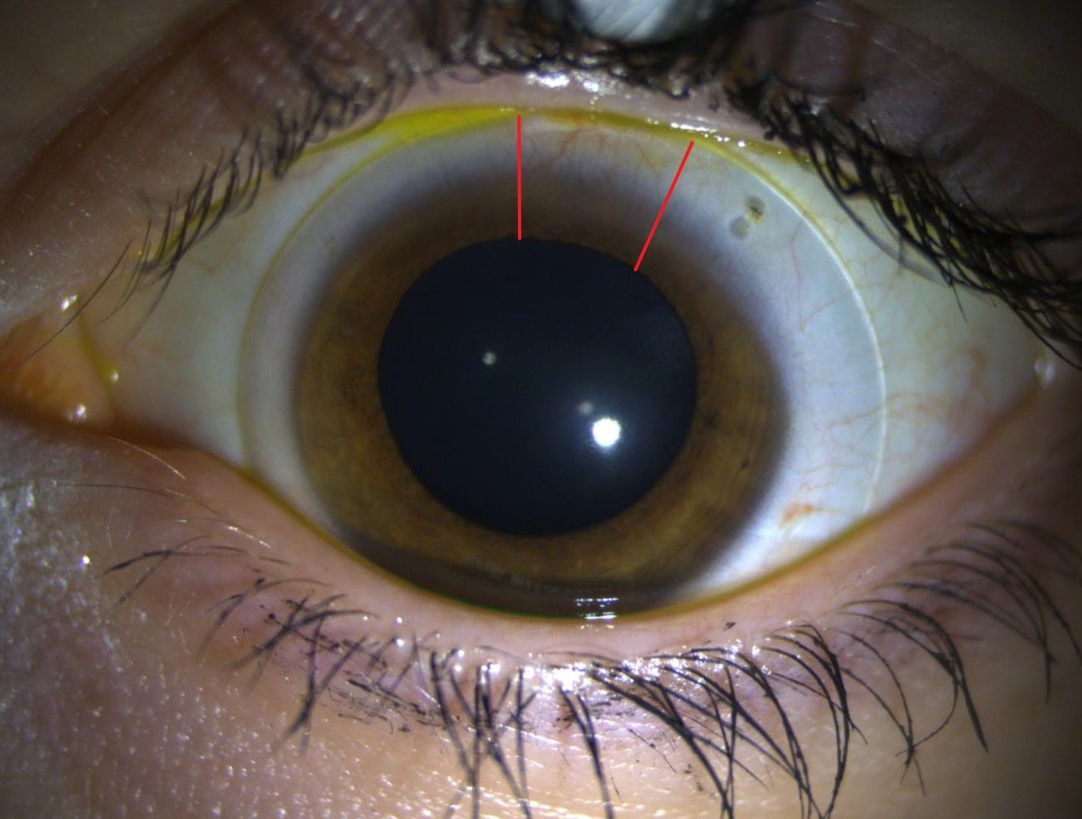
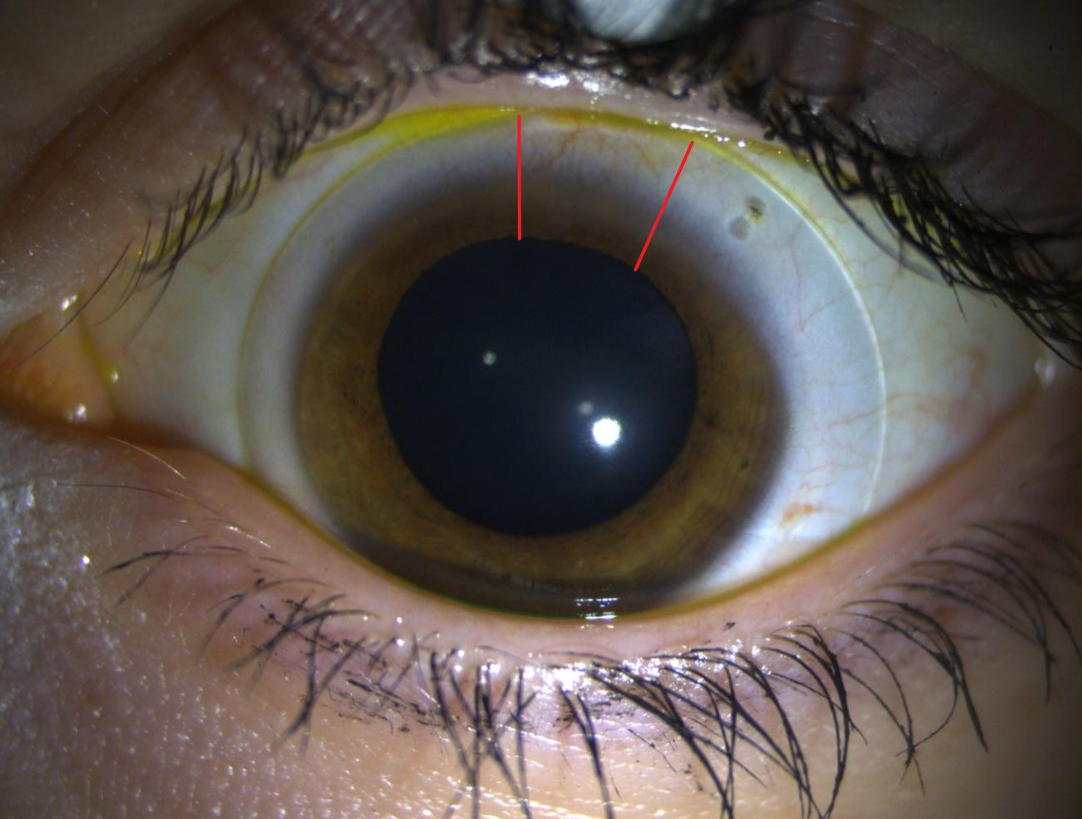
Figure 2. This photo, taken by slit lamp external photography, shows our patient’s left lens at final dispense. The red lines outline the SmartChannel™ that was added to increase oxygenated tear exchange at the superior limbus. The channel is 30 degrees wide with a 0.15um depth.
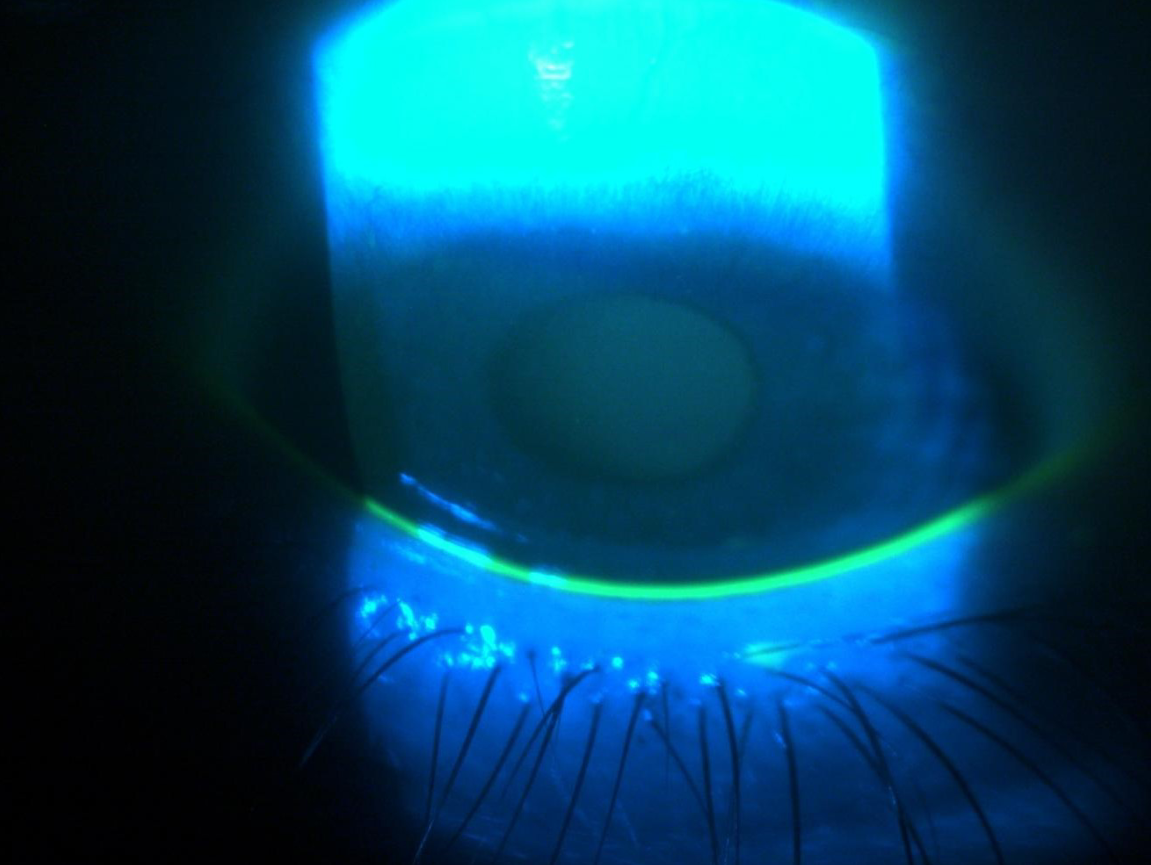
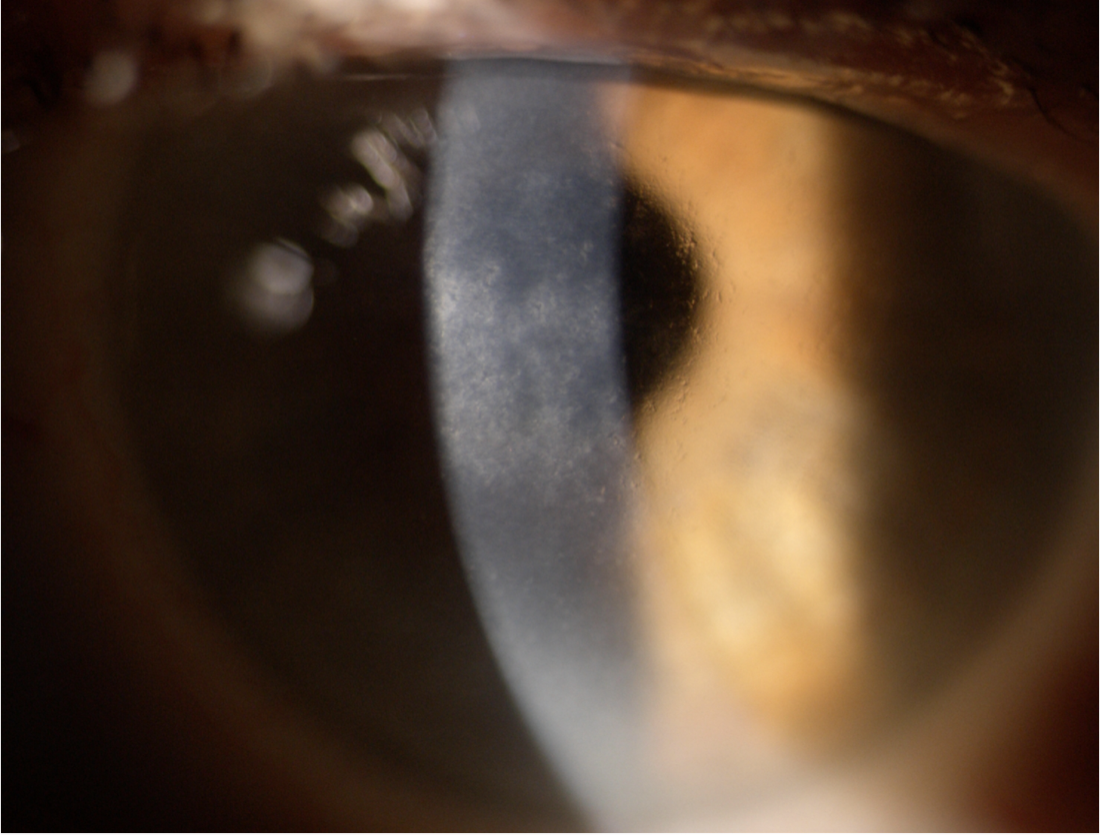
Figure 3. This photo, taken by slit lamp external photography, shows the patient’s ocular surface OS at their most recent follow up appointment. As you can see, the whorl-like fluorescein pattern has completely resolved leaving trace residual haze at the superior limbus.
Conclusion
Contact lens induced LSCD is multifactorial. Contact lenses disrupt the tear film, cause hypoxia and mechanical trauma leading to an inflammatory response.4
LSCD is typically bilateral and asymmetric, but in this case it was unilateral. The patient is at higher risk of developing LSCD in the fellow eye, so you must monitor it closely. To maximize our patient’s ocular health, we switched her into a daily disposable lens and monitored every few months.3
Ensuring that soft contact lenses are properly fit helps to minimize the risk of developing LSCD. As a fitter we should aim for lenses with a low modulus, high DK, and adequate movement (0.1mm-0.4mm). Keep in mind that, although popular, silicone hydrogel lenses have shown increased mechanical trauma due to the decreased flexibility needed to achieve increased oxygen permeability.2
Educate patients on wear schedules, emphasizing no extended or overnight wear. Pay special attention to those with steeper corneas and tighter lids because they are prone to more friction and damage due to inadequate lens movement.4
More conservative treatment options should be explored prior to using scleral lenses to manage LSCD. This typically begins with the cessation of contact lens wear, preservative-free artificial tears, lid hygiene, warm compresses, punctual plugs and other measures as indicated. To address possible inflammation, consider adding topical steroids and/or topical cyclosporine to the treatment plan.4
Surgical management may be considered when all other options are exhausted due to potential risks and complications. Surgical options include, but are not limited to, epithelial debridement, amniotic membrane transplantation and limbal stem cell transplantation.3
1. Cheung AY, Sarnicola E, Denny MR, Sepsakos L, Auteri NJ, Holland EJ. Limbal Stem Cell Deficiency: Demographics and Clinical Characteristics of a Large Retrospective Series at a Single Tertiary Referral Center. Cornea. 2021 Dec 1;40(12):1525-1531.
2. Dumbleton, Kathy M.Sc., M.C.Optom, F.A.A.O.. Noninflammatory Silicone Hydrogel Contact Lens Complications. Eye & Contact Lens: Science & Clinical Practice: January 2003 – Volume 29 – Issue 1 – p S186-S189
3. Lee SC, Hyon JY, Jeon HS. Contact Lens Induced Limbal Stem Cell Deficiency: Clinical Features in Korean Patients. Korean J Ophthalmol. 2019 Dec;33(6):500-505
4. Rossen J, Amram A, Milani B, Park D, Harthan J, Joslin C, McMahon T, Djalilian A. Contact Lens-induced Limbal Stem Cell Deficiency. Ocul Surf. 2016 Oct;14(4):419-434.